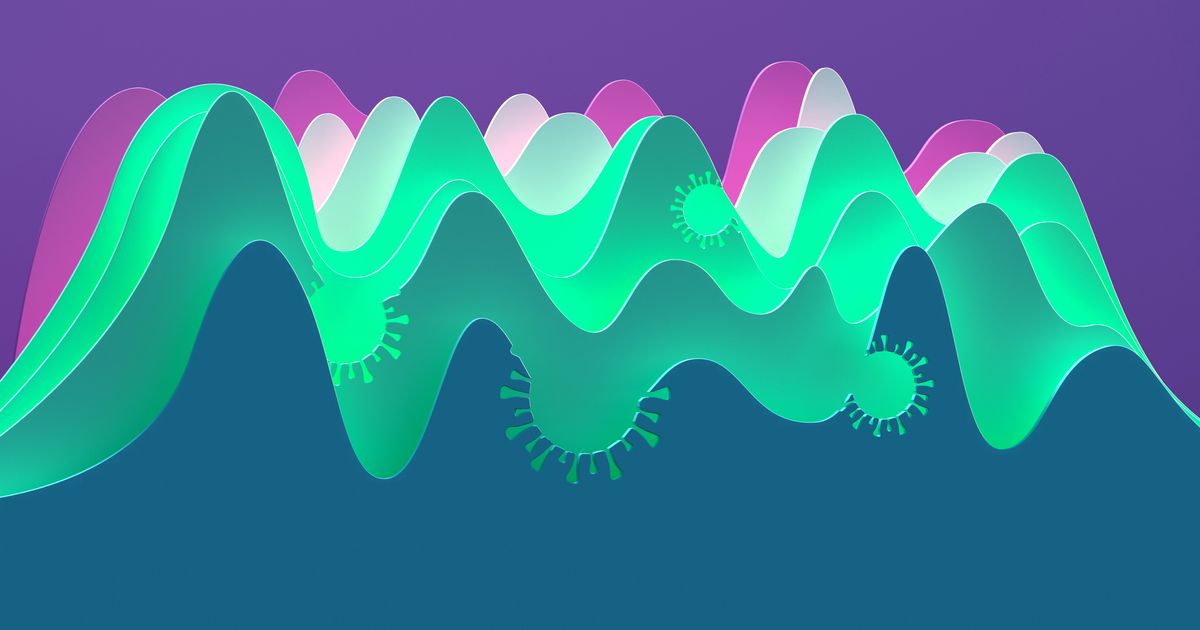
The news of an emerging COVID-19 variant or subvariant is alarming — and rightfully so. COVID completely upended our lives and has killed more than 1 million Americans since 2020. It’s hard not to worry when you hear about a new ― and often more contagious ― strain of the virus.
The latest concern comes from news about subvariants including BA.2.75, BA.2.75.2, BF.7 and BA.4.6, all of which have appeared in headlines in recent weeks and will likely be topics of concern in the coming weeks, too.
But it’s also important to remember that as COVID continues to infect people, it will also continue to evolve. In fact, according to Dr. William Schaffner, a professor of preventive medicine in the department of health policy at Vanderbilt University Medical Center, “the World Health Organization has a worldwide surveillance mechanism underway that keeps looking for new strains of [COVID-19] and new strains of influenza.”
This radar system keeps track of emerging variants and subvariants so experts can see if they are becoming prominent enough to be a concern, he noted. Many of these new strains amount to nothing while others (like BA.5) turn into dominant forces that infect hundreds of thousands of people.
Below, experts share what you need to know about the latest omicron subvariants:
New variants and subvariants are emerging all the time, and that’s just a normal part of a virus’s progression.
It’s normal for viruses to evolve into new variants and subvariants over time. Viruses “generate a lot of change as they replicate in our body, and any changes that provide them with a benefit in terms of the ability to transmit from one person to another will stick around,” said Dr. Catherine Blish, a professor of infectious diseases at Stanford Medicine.
In the end, viruses want to be as contagious as possible and spread to as many people as they can. Lately, RNA viruses (like COVID-19) are evolving at a faster rate, Blish said, which is why we are seeing new variants and subvariants pop up multiple times throughout the year.
It’s not known if new subvariants will cause a spike in cases.
Relatively speaking, new omicron subvariants like BA.2.75, BA.2.75.2, BF.7 and BA.4.6 account for a small percentage of cases right now — though BA.4.6 has been increasing throughout the United States, and it currently accounts for about 13.6% of cases, according to the Centers for Disease Control and Prevention. BF.7 makes up about 4% of current cases.
But, as you’re probably well aware, things change quickly with COVID. “It’s too early to say whether BA.2.75.2 or even the parental BA.2.75 is going to really take hold,” Blish added.
She noted that in the past, potentially worrisome variants have appeared but then quickly disappeared. “Nobody thinks about lambda and mu, and those were other variants that [came] up, but they didn’t have enough of a survival advantage to persist,” she said. That can also hold true for subvariants.
The new omicron subvariants do appear to be just as contagious as previous omicron strains.
According to Schaffner, the new variants “are quite similar to their virus parents, but they may have slightly altered characteristics.” He added that, as of now, the subvariants that are currently circulating have only minor differences from the dominant strains.
For BA.275.2 particularly, “it is spreading, [and] it seems to be at least as contagious as our current BA.4 and BA.5 subvariants, maybe even more so,” Schaffner said, but it’s too early to be completely sure.
Additionally, some very early lab studies show that, though the current vaccines continue to protect against severe disease, hospitalization and death, BA.275.2 may be able to evade some of the protection of the current vaccines, Blish and Schaffner both said. This may mean people who get vaccinated or boosted can still get infected but will likely only end up with a mild infection.
Blish stressed that early lab data doesn’t always translate to the real world, so this is something experts will monitor in the weeks and months to come.
Images By Tang Ming Tung via Getty Images
The new subvariants don’t seem to be causing more severe illness.
“The coronavirus variants we’re dealing with now seemingly produce milder infections,” Schaffner said.
He added that these strains are very contagious and do cause a lot of mild infections, including in people who have been vaccinated or previously infected, but people aren’t getting as sick as they were a year or two ago.
This is because of the vaccines and boosters, antivirals like Paxlovid and a large amount of immunity from previous infections, previous vaccinations or a combination of both.
Though most infections seem to be milder, there is still the risk of developing “long COVID,” which can mean you have lingering symptoms for weeks, months or even longer. Experts don’t know exactly why long COVID develops, but it is more common in people who had severe infections and also tends to be more common in people who are unvaccinated.
As of now, BA.4 and BA.5 are still the dominant subvariants.
Currently, BA.4 and primarily BA.5 are the dominant COVID-19 strains throughout the country, meaning they make up most of the cases right now — though BA.5 cases are waning (but it still makes up nearly 80% of cases in the U.S.).
“We have to recognize that we have a more immediate threat,” Schaffner said, and that immediate threat is the current dominant omicron subvariants. “They’re the ones that are right in front of us ready to bite us in the nose,” he added.
If there is a rise in cases in the near-term future, it will likely stem from them, Schaffner suggested. “We have to protect ourselves against [the current strains] while we keep an eye on the others.”
Winter could bring a rise in cases as more people stay indoors.
“I have significant worry that as people move inside with the colder weather we’re going to see an increase in cases,” Blish said. “The best thing we can do is to get more people vaccinated with this new booster.”
The new bivalent booster shot was specifically created to target the omicron strain, particularly BA.4 and BA.5, which remain dominant. The booster is available to everyone older than 12 — though, young people ages 12 to 17 need to get the Pfizer booster. The Moderna booster is authorized only for those 18 and older.
Things like preexisting immunity from vaccinations and illness can certainly help protect people from getting very sick, too, but the bivalent booster remains the best way to increase immunity that much more. It also helps protect those who are immunocompromised or unable to get vaccinated.
“My hope is we will not see the huge surge in hospitalizations that we’ve seen in the past, but that really relies on people updating their boosters to a certain extent,” Blish said.
Experts are still learning about COVID-19. The information in this story is what was known or available as of publication, but guidance can change as scientists discover more about the virus. Please check the Centers for Disease Control and Prevention for the most updated recommendations.